Understanding Dry Eye
Find out about what the Tear Film does and the different types of Dry Eye diseases.
Home » Services » Dry Eye Management » Treatment Options for Dry Eye
The treatment we prescribe or recommend for you will be influenced by the results of your specific dry eye assessment and targeted towards the form of dry eye disease you are diagnosed with.
It is important to understand that in many cases the treatment options for dry eye will enable you to manage but not necessarily cure the disease, so ongoing and repeated attention is frequently required. In some cases treatment may not result in significant improvement in symptoms, but is important to prevent progression of meibomian gland disease and of your dry eye condition worsening further.
For all dry eye sufferers there are a number of relatively simple and inexpensive strategies for the reduction and management of symptoms. These include:
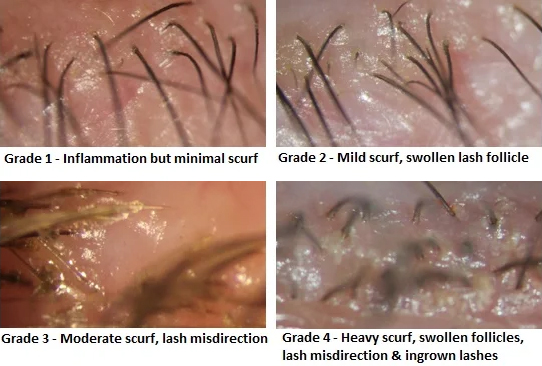
If anterior blepharitis is detected, this should generally be addressed prior to the commencement of other dry eye therapy. The mainstays of treatment for anterior blepharitis include:
Dry eye from aqueous insufficiency arises from reduced secretion of the lacrimal gland and causes tear hyperosmolarity, where the concentrations of tear salts and proteins become abnormally high. In turn this causes inflammation of the ocular surface, damage to the epithelial cells at the front of the eye, and an unstable tear film. Aqueous insufficiency is treated with some of the following :
As around 80% of cases of dry eye are evaporative due to mybomian gland dysfunction, this condition frequently requires treatment. Treatment strategies are aimed at either increasing the quantity of oils (meibum) produced by the glands or, more usually, unblocking glands and ensuring the free flow of oils from them. This typically requires the application of heat to “melt” and reduce the viscosity of old thickened oils remaining in the glands before mechanically expressing them. This may need to be repeated a number of times before satisfactory gland function is restored. Some of the treatments outlined above for aqueous insufficiency are also of use in treating evaporative dry eye.
Once the meibomian glands have been heated, there are a number of techniques and instruments that can be used to express the glands. Two examples are expression with forceps and expression with Mastrota Paddle. Although occasionally we employ forced expression of the glands like this to assess the quality of the meibum, generally we now use this relatively infrequently for treatment; even then, very gently rather than with significant force. Other methods for treating meibomian gland dysfunction include:
Whereas LipiFlow® typically involves only a single treatment followed by a review a few weeks later, the eye-light® LLLT and OPE IPL require at least two and up to four treatment sessions conducted five to ten days apart. Reviews are typically scheduled a few weeks after treatment has been completed, or at any time you feel a need to return.
Because your tear function will have been quantified objectively prior to treatment, improvements can be clearly demonstrated at subsequent reviews using the same tests that were conducted at your initial dry eye assessment.
For a copy of this page in handout form click here.
Find out about what the Tear Film does and the different types of Dry Eye diseases.
Learn about the technologically advanced way that Collins Street Optometrists diagnose and assess Dry Eyes
Other links and resources you can use to find out more about Dry Eye diseases.
Monday - Friday
9AM - 6PM
Saturday - Sunday
CLOSED